The terms ON and OFF have been used to describe responses to Levodopa therapy for over 40 years. However, to this day, there’s still no universally agreed upon definition for the term OFF.
This poses a problem for the doctors who are expected to recognize it and the people living with Parkinson’s who try to describe it.
When both sides interpret OFF in different ways, it often means that people with Parkinson’s don’t get the interventions or treatments they need to reduce their OFF periods and live well with Parkinson’s.
In an attempt to help you become a better advocate for yourself, this article will highlight four different types of OFF and why they happen. We will also offer a list of questions and a working definition of OFF that you can take with you to your next doctor’s visit. (P.S. You can share your experiences of being OFF with us by completing this short survey.)
What Is OFF?
The simplest definition of OFF is a period when your medication (Carbidopa/Levodopa) is not working optimally and your motor and non-motor symptoms return.
But there’s more nuance to it than that, so we’ll delineate between the four types of OFF.
- Delayed ON
This is what happens when it takes longer for your medication to start working. Often this is the first dose you take after a long night of sleep or after a meal. In particular, after a high protein meal that may block the absorption of your medication. - Wearing OFF
This is what happens when your medication wears off before it’s time to take your next dose. This happens more frequently as your Parkinson’s progresses. - Unpredictable OFF
This is when your symptoms return unexpectedly and there seems to be no relationship to your dosing schedule. - Dose Failure/Partial ON
This happens when symptoms subside after you take your medication, but not as much as they usually do.
What types of symptoms might you experience when you're OFF?
Being OFF is more than just having a bad day. It involves experiencing a host of motor and non-motor symptoms that you have come to expect your medication to control.
While the number and severity of symptoms differ for everyone, here are the most common ones people experience when they are OFF:
Motor Symptoms of OFF
- Rest tremor
- Bradykinesia
- Rigidity
- Muscle cramping
- Reduced dexterity
- Slowness
- Balance issues
- Swallowing
- Hypophonia
- Shortness of breath
- Dystonia in hands, feet or legs
Non-Motor Symptoms of OFF
Many non-motor symptoms remain present in the ON state, and they do not respond to dopaminergic treatment. Therefore, you would not be considered OFF if those remain present. However, there are some non-motor symptoms that worsen or are more severe in the OFF state. These often include:
- Fluctuations in cognition, attention, anxiety, depression, apathy
- Sweating, lightheadedness, abdominal pain, bloating, urinary issues
- Visual disturbances, pain, dysesthesia, akathisia, restless legs syndrome
How many people living with Parkinson's experience OFF periods?
It has been reported that within one to two years of beginning levodopa therapy, almost 50% of people with Parkinson’s notice that their medication lasts for shorter periods of time. Initially, this was why some doctors choose to delay prescribing Levodopa, a still unresolved debate.
The debate in itself is not the problem at hand, however. The problem is that half of the people living with Parkinson’s are experiencing OFF periods and many of them are not getting the relief they need.
Here are five ways you might be able to change that in order to get the best care for you.
#1 - Ask Questions
Your appointment time with your doctor is limited, and unless they prompt you to discuss OFF in a specific way, you may miss some key information about your medication and how it is supposed to work. Take these questions with you the next time you go to get the conversation about OFF started.
- How long should it take my medication to start working?
- Should my medication be working the same throughout the day?
- What should I do if my medication begins to wear OFF before my next dose?
- What if I take a dose and nothing happens?
- Can I take my medication when OFF symptoms occur, even if it’s not time for my next dose?
#2 - Request an Assessment
There are several assessments (WOQ-32, WOQ-19, WOQ-9) used to assess the frequency, severity and timing of OFF periods. They’ve often been used by those researching OFF; however, they might also be helpful as a way for you to track your experience and share it with your doctor.
Your movement disorder specialist (MDS) is likely familiar with these questionnaires already; however, if your Parkinson’s doctor is a general practitioner, they may not be familiar with this tool. In that case, completing the questionnaire and bringing one to each of your appointments may be a great way for you to track your OFF periods over time and help your doctor get the full picture of your experience.
#3 - Keep a Diary
If you prefer a more fluid way of tracking your OFF periods, keeping a diary may be the best fit for you. If you go this route, be sure to include:
- Medication dose
- Timing
- The severity of symptoms over time
- How the symptoms impact your quality of life
- Any side effects you experience
#4 - Take a Care Partner
One of the best ways to ensure you get the most out of the limited time you have with your doctor is to bring a care partner or friend with you to every appointment. Have that person record the appointment on their phone. This frees both of you up to ask questions and report on what’s been happening between appointments. It also allows you to relax and not stress about having to remember everything your doctor says.
Once you return home, listen to the recording together and write down key actions you need to take between now and your next appointment.
#5 - Come to a Common Definition of OFF
This is perhaps the most important action you can take to navigate and hopefully minimize OFF periods. When it comes to a definition of OFF, you don’t have to agree with the rest of the medical community, you just have to agree with your doctor and care team.
For example, your doctor might not think that predictable wearing off is equivalent to an OFF state. You might think it is. In order to account for differences in how you define OFF, it’s important to determine what OFF means to both of you. And to come up with a working definition together. You might even have a code such as, “When I say X, I mean Y.”
You have Parkinson’s, so chances are, you’re going to be seeing your doctor on a regular basis for many years to come. The earlier you can establish a language for how you talk about OFF, the better chance you have of getting the interventions and treatment you need to live well with Parkinson’s.
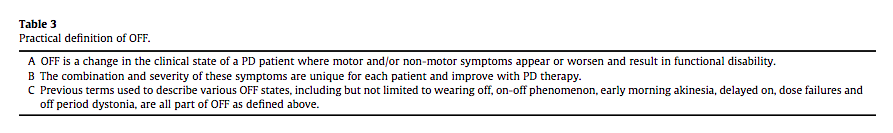
As a starting point, here’s a working definition of OFF developed by Chou et al.
To download this post as a PDF, click here.
Do You Have an OFF Story to Share?
This post is the first in a series about what it means to be OFF. If you have a story about OFF and what you’ve done on your own and with your doctor that has helped you to minimize or navigate these periods, and you’d like to share it with us, please send us an email at blog@dpf.org.
This post was written by the Davis Phinney Foundation.
This blog series is sponsored by Sunovion Pharmaceuticals Inc.









