We receive emails every day from people wondering who they should see for a wide variety of issues that often go hand-in-hand with Parkinson's. Since it comes up often enough, we decided to create a guide that answers exactly that.
To put this piece together, we gathered up the 15 most frequently asked questions we've received from our community members via email, text, and in-person chats. We hope this Q&A will be helpful to you along your path with Parkinson's.
"My medication is not working. (It doesn't last long enough. I have too many OFF times a day. I feel nauseous.) Who should I see?"

If you have a movement disorder specialist (MDS), make an appointment to see them. If you don't have an MDS, find one in your area. We know that the MDS closest to you isn't always geographically convenient; however, if you have Parkinson's, having one on your medical care team can be the difference between living well with Parkinson's and just getting by.
Your MDS is the person on your medical care team who has the most familiarity with the full spectrum of Parkinson's medications and treatments. They see thousands of people with Parkinson's every year; so, they have probably helped people with issues similar to yours before.
When it comes to primary care doctors or even neurologists, they may know very little about potential Parkinson's medications beyond Carbidopa/Levodopa. Also, they just don't have the experience of seeing people with Parkinson's every day; so, their ability to notice, identify, and treat the myriad of issues you could potentially face during your time with Parkinson's is significantly lower than an MDS. We know many people who drive three to four hours or even fly to see their MDS, and they say it's worth every penny and every minute.
So, the first order of business is to find an MDS. The next step is to begin tracking your symptoms with as much detail as possible. Think of your medication as being one spoke on a wheel, but for it to work as well as it can, the other spokes (food, exercise, sleep, energy, mindset, etc.) must work as well. Therefore, consider tracking the following each day:
- Nighttime hours of sleep (good and inadequate sleep)
- Daytime naps and sleepiness
- Drops in energy throughout the day
- Spikes in energy throughout the day
- Minutes of exercise, and the time of exercise
- Mood
- Physical issues (nausea, constipation, bladder, etc.)
- OFF times
- ON times
- Medication intake, dosage, and timing
- Other, non-Parkinson's medication, dosage, and timing
- Anything else of consequence like hours of work, travel, stress, etc.
Take this tracking information with you to your next doctor's appointment.
In the meantime, watch this great interview with Dr. Karunapuzha. He talks about how Parkinson's medication works and what you can do to get the most out of each dose.
Other questions an MDS can help you with:
- Are there any new drugs in the pipeline that might be able to help me with X?
- Are there any clinical trials in the area you think I'd be a right candidate for?
- My dystonia, tremors, balance is getting worse. What can I do?
- Is it okay to exercise with nOH?
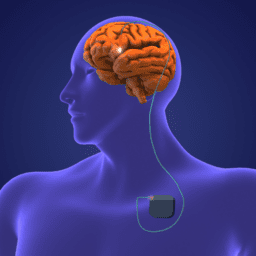
- Am I a good candidate for Deep Brain Stimulation (DBS) or Duopa™?
"How much do pharmacists know about Parkinson's, and what can they help me with?"
Because Parkinson's is something you will probably have for a very long time, you and your care partners will see your pharmacist regularly. And, because they will know all of the medications you take, those that are related to Parkinson's and those that aren't, they will be on the lookout for medication interactions that your primary doctor may not always be aware of.
Whenever you’re prescribed a new medicine, be sure to ask your pharmacist if there's anything you need to know about how it might interact with other meds you're taking. Not all interactions are severe; however, some may cause minor issues that you can avoid if you know about them upfront.
Other questions a pharmacist can help you with:
- Can I crush up my pill and take it in my food or beverage?
- Can I cut the pill and take half now and half later?
- Can you put my pills in a bottle I can open more easily with my tremor?
- How much time do I need to wait between taking pill A and pill B?
"I'd love to try CBD because everyone in my support group is talking about it. I don’t know where to start or what dosage to take. Who should I see?"
Questions about CBD are some of the most challenging questions we receive because there are very few medical professionals who know enough to help you. The truth is, the science just isn't there yet, and while anecdotal evidence can sound exciting, there isn't a "recommended" dose or type that works for everyone, or anyone.
We do recommend starting with your MDS because they may be following the research and clinical trials that involve CBD and Parkinson's. However, many MDSs don't recommend it because its efficacy is still unproven.
If you don't have an MDS, speak with your primary care doctor and pharmacist before you add it to your daily regimen. Hopefully, as more and more people study it, there will be more clarity about what to use it for, how it works, who it works for, and what symptoms it can help for those living with Parkinson's.
"I'm noticing that I feel down a lot. Or I don't feel as sharp as I used to be. I know there's stuff I could be doing, but I can't seem to act. Who should I see?"
Several things could be going on here. You might be feeling depressed, you may be experiencing cognitive decline, which is causing you to feel sad, or your body might not be responding well to your medications, and it's making you feel tired and uninterested in activities you used to care about.
An excellent first step is to get evaluated by a neuropsychologist who specializes in neurological disorders. A neuropsychologist is someone who specializes in the relationship between behavior and brain function. Cognitive impairment (CI) and behavioral complications such as depression, anxiety, and apathy can be some of the earliest symptoms people with Parkinson's notice, often before they even get an official diagnosis. Most people with Parkinson's will experience these issues at some point.
A neuropsychologist will evaluate your thinking skills, including memory, attention, reaction time, language, and visual perception. They will also assess your emotional functioning. Your results will then be combined with the rest of your medical record to help your neuropsychologist develop a diagnosis and recommendations for improving your quality of life. One of the benefits of getting an evaluation like this early on is that then you will be able to see how your Parkinson's is progressing over time and act as soon as possible to manage your symptoms.
You can access a list of board-certified clinical neuropsychologists via the American Academy of Clinical Neuropsychology website here.
Where your neuropsychologist may refer you based on your clinical assessment results:
- Mental health provider such as a licensed clinical psychologist, a licensed professional counselor (LPC), or a licensed clinical social worker (LCSW) who specializes in working with people with Parkinson's and can provide different types of therapy for issues such as depression, anxiety, apathy, etc.
- Occupational therapist
- Speech-language pathologist
- Rehabilitation specialist
- Clinical neuropsychologist to work on maintaining or increasing cognitive skills, executive function, overall cognitive ability
To watch one of our most popular videos on the non-motor symptoms of Parkinson's, The Parkinson's You Don't See: Cognitive and Non-motor Symptoms with neuropsychologist Joanne Hamilton, click here.
"I'm in pain a lot. Some people tell me that's just because I'm getting older. But it's getting in the way of living my life. Who should I see?"
Pain is a common symptom of Parkinson's, but many people don't seek treatment for it because chronic pain is often considered the price of getting older. However, there is pain that is unique to people with Parkinson's, including:
- Pain due to rigidity or arthritis pain that can be exacerbated by Parkinson's (musculoskeletal pain)
- Dystonic pain (curling of the toes and/or fingers)
- Nerve pain (this can be exacerbated if you also have a stooped posture)
- Central pain
If you are experiencing significant pain, it's essential to see a neurologist. Sometimes your pain will present as one thing but be the result of another medical issue. It's important to determine what the pain is or isn't so your doctor can plan the best possible treatment for you.
Other questions a pain specialist or neurologist can help you answer:
- Do men and women with Parkinson's experience pain in the same way?
- What's the link between depression and pain?
- What activities help reduce pain? Is exercise good for minimizing or eliminating pain?
- Are there any complementary or alternative therapies that have been proven to help reduce pain?
- What types of medicine work for different kinds of pain?
"I'm having a lot of trouble sleeping. Who should I see?"
Sleep disturbances are the most commonly reported non-motor symptom of Parkinson's, and very often, they occur long before someone receives an official diagnosis.
Over the years, we've addressed everything from REM Sleep Behavior Disorder (RBD) to sleep hygiene, insomnia, fatigue, sleepiness, and more. Still, most people are not getting enough sleep, and unfortunately, just knowing you should get better sleep isn't enough to make it happen.
Lack of sleep can put people at higher risk of:
- Depression
- Pain
- Falling and other accidents
- Cognitive decline
- Developing comorbidities
So, it's important to talk to a neurologist who specializes in sleep if you have access to one. If not, a general neurologist is the next best option.
Like pain, many people think lack of sleep it too ubiquitous to count, so they don't bring it up during appointments; however, it plays such a critical role in your quality of life that the sooner you address it, the better.
Common sleep issues a sleep specialist can help you with:
- Insomnia
- Sleep fragmentation
- Excessive Daytime Sleepiness (EDS)
- Nighttime sweating
- Trouble moving in bed
- Sleep apnea
- Fatigue
- Restless Leg Syndrome (RLS)
"I was recently diagnosed with Parkinson's and am only experiencing a few symptoms. My life hasn't changed, and I'm still active. Still, someone in my support group told me I should see a physical therapist as soon as possible. Why should I do that if I don't have any issues yet?"
Most people are aware that doing physical therapy (PT) can help improve balance, reduce the risk of falling, improve the ability to walk faster and farther, and improve quality of life. But there are a variety of other daily tasks physical therapy can help you with such as:
- Getting in and out of bed
- Turning over in bed and pulling yourself up
- Getting down on the floor and getting back up
- Getting in and out of the car
- Walking around the grocery store or shopping (PT can help you improve your ability to multi-task)
- And whatever other activities of daily living you want to keep doing
But, the reason it's important to work with a PT before you think it's time, is because you can begin doing the exercises that will address your current weaknesses so that you stay stronger and mobile for longer. You may ride your bike every day or still run multiple marathons a year; however, there's a good chance you still have some gaps in your flexibility or mobility that PT could close. Also, by getting an assessment early, your PT will be able to see how your Parkinson's is progressing over time so they can give you exercises to address areas that may be getting weaker.
Seeing a physical therapist for an assessment now doesn't mean you have to go all the time. We know many people who get a PT assessment as soon as they are diagnosed and then work on their program at home or at their gym for years before they go back. Parkinson's is a progressive disorder, so the better you can track your strength, mobility, and flexibility markers along the way, the better equipped you will be to address issues when they are new and keep them at bay for as long as you can.
If you don't yet have a physical therapist, you can find one in your area here.
Common issues a Parkinson's physical therapist can help you with:
- Balance problems
- Arm swing
- Lack of coordination
- Fatigue
- Pain
- Gait
- Immobility
- Weakness
"Every day I hear people talking about the latest and greatest diet that is good for Parkinson's. It's hard to keep track of all the conflicting information. Who should I see?"
When it comes to nutritional plans, what works for you may not work for someone else. And for every article (peer-reviewed or otherwise) on why diet X is the best, there is another one that claims Y is the best. To find the best nutritional strategy for you, see a registered dietician (RD) who specializes in working with people with Parkinson's or other neurological disorders.
RDs are usually the most qualified health professional out there on the topics of nutrition and dietetics unless your primary care doctor, neurologist, or movement disorder specialist specializes in that field. If you don't have access to an RD in your area, you can check out some of our resources on nutrition.
Other issues an RD can help you with:
- Nutritional treatments for Diabetes or high/low blood pressure
- Digestive issues, constipation, bloating, abdominal pain (see a Gastrointestinal (GI) if the problem is serious and chronic)
- Weight gain/loss
- Nutrition for exercise performance
- Meal planning
"I get more and more headaches. I have a cough that won't go away. I don’t know if they’re because I have Parkinson's or because of something else. Who should I see?"
These could be related to Parkinson's, but they may not be. Work with your primary care doctor first, and if they can't help you, they can refer you to someone who can.
"It's getting difficult to button my shirts, write checks, make coffee, do household chores, etc. I'm not ready to lose my independence or hire someone to help me with them. Who should I see?"
Occupational therapists (OTs) are your go-to person in this situation. They help people across the lifespan do things they want to do through the use of therapeutic activities.
Their interventions focus on:
- Adapting your environment through modifications (sometimes small changes in design make a big difference)
- Modifying tasks
- Improving cognitive function
- Teaching new skills or ways of doing something
- Educating you and your care partners, family members, or friends so they know what you can and can't do so you can maintain as much of your independence as possible
- And more!
Other ways an OT can help improve your quality of life:
- Assess your home at different stages of your Parkinson's and offer ideas of how to make your living area safe
- Simple strategies to make it possible to continue doing activities of daily living (ADLs) for as long as possible
- Tremor management
- Stretching
- Toileting
- Eating
- Transfer training
- Bathing
- Using adaptive equipment
- Improving functional mobility
- Care partner training
"I notice my voice is getting softer, and sometimes even though I have something I want to say, I don't because I'm embarrassed, or I don't want to frustrate people. Who should I see?"
A soft, quiet voice is one of the most common complaints among people with Parkinson's. The good news is that your ability to speak and be heard can be improved.
Consider working with a speech-language pathologist (SLP), ideally, one with specialized training in working with people with Parkinson's. Although it's easier to reverse speech challenges early on, it's never too late to benefit from this type of training.
If your healthcare team does not have any recommendations and your network doesn't yield any names, here are a few ideas to get you started.
LSVT® LOUD is a well-established speech-language pathology program for Parkinson's. They have a "Clinician Finder" tool on their website that you can use to find SLPs who are certified in LSVT® LOUD near you. SPEAK OUT!® is similar to Parkinson Voice Project, which also has a Clinician Finder tool that allows you to enter your ZIP code and find nearby SLPs who have gone through training to offer SPEAK OUT!®
Other issues a speech-language pathologist can help you with:
- Eating
- Swallowing issues
- Saliva management
- Dry mouth
- Drool
- Cognitive complications (losing your train of thought, thinking skills)
- Starting an action
- Problem-solving
"Is it true that people with Parkinson's are at higher risk of getting melanoma? Who should I see?"
While several studies have shown that people with Parkinson's are at a lower risk of developing most cancers, people with Parkinson's are at an increased risk of melanoma. The reverse is also true; those who have melanoma are at an increased risk for Parkinson's.
So, while getting an annual skin check beginning around age 20 or 30 is recommended for everyone, if you have Parkinson's, it's even more critical. Yearly skin exams can help detect cancer at its earliest and most treatable stages. They also allow your dermatologist to find and remove precancerous lesions before they develop into skin cancer.
Just be sure that you go to someone who does a thorough, head-to-toe skin exam that includes checking your scalp, fingers, toes, fingernail and toenail beds, and everywhere in between. Also, be sure to tell them you have Parkinson's and point them to research on the link between Parkinson's and melanoma if they don't know about it. Not everyone will.
Other issues a dermatologist can help you with:
- The health of your hair, nails, and mucous membranes
- Acne
- Dermatitis and eczema
- Fungal infections
- Psoriasis
- Rosacea
- Shingles, or herpes zoster
- Warts
"I'm having more trouble reading these days. Is this Parkinson's or just my eyes aging? Who should I see?"
Your issues may be related to the aging of the eye, but there are several issues related to vision that are unique to people with Parkinson's. So, if you go to your general ophthalmologist, but the problem isn't solved with new (or first) lenses, ask for a referral to a neuro-ophthalmologist. Neuro-ophthalmologists are ophthalmologists or neurologists who have received specialized training so they can diagnose and treat vision issues that are the result of neurological diseases.
Vision issues a neuro-ophthalmologist can help you with:
- Eye movement issues that impact reading, depth perception, ability to focus, etc.
- Blinking abnormalities
- Dry eyes
- External eye disease
- Color vision deficits
- Visual disturbances
- General eye diseases such as cataracts, glaucoma, macular degeneration
Here's a webinar on vision problems and Parkinson's put on by The Michael J. Fox Foundation.
"I never had problems with my teeth until I got Parkinson's. Why am I having issues now? Who should I see?"
Managing dental health and Parkinson's is an integral part of living well. Regular dental care can minimize your risk of experiencing pain and discomfort. Still, most importantly, it can reduce the risk of infection, which can be a significant stressor on the body when coupled with Parkinson's-related challenges.
Some of the issues that cause dental problems in those with Parkinson's include:
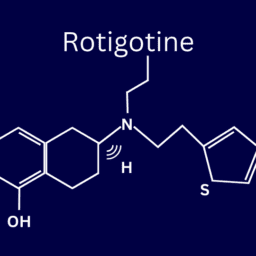
Medication - Medications may cause a decrease in the production of saliva or dry mouth (xerostomia). Saliva helps prevent tooth decay by neutralizing acids produced by bacteria in your mouth as well as by washing away food debris in your mouth. Dry mouth is a common side effect of anticholinergic medications, Carbidopa/Levodopa, and related Parkinson's medications. Dry mouth may also occur with the use of medications prescribed for depression, anxiety, sleep issues, urinary issues, and orthostatic hypotension. However, your dentist may be able to treat it.
Treatments - Botulinum toxin (Botox® ) injections to control drooling (sialorrhea) can sometimes be so effective at reducing excess saliva production that it results in dry mouth. Be sure to tell your dentist if this is the case.
Motor control - Decreased fine motor control, reduced hand strength, and slow movements (bradykinesia) associated with Parkinson's can make flossing and brushing teeth difficult. As well, stiffness associated with Parkinson's (rigidity) can lead to less effective tooth brushing movements overall. Those who experience motor side effects from medications like involuntary twisting (dyskinesias) may also have difficulties performing proper oral care regularly.
Be sure to talk about these issues with your dentist and medical care team so you can find solutions and maintain good oral health.
If you need help sticking to a routine, consider doing this simple, daily, oral-hygiene plan.
It also may be a good idea to get any oral surgery you may need early in your journey with Parkinson's as it may be more challenging to do so as your Parkinson's progresses. Tell your dental care providers that you have Parkinson's and always disclose medications you're taking as MAO-B inhibitors can be problematic if you receive anesthesia.
"I'm young and will have to work for as long as I can since I am the sole breadwinner in my family. I haven't told anyone at work, but when it's time, will they have to make accommodations for me? Who should I see?"
When Parkinson's reaches later stages, it is considered a disability. In that case, the law requires employers to make reasonable accommodations for employees. If you’re worried about what this will mean in the future, or you have concerns about your ability to continue working in your current role, seek the advice of an employment lawyer.
What Have We Missed?
Do you have a question we didn’t address here? If so, please leave it in the comments, and we’ll do our best to answer.
Want More Practical Articles Like This?
Much more can be found in our latest edition of Davis Phinney Foundation’s Every Victory Counts® manual. It’s packed with up-to-date information about everything Parkinson’s, plus an expanded worksheets and resources section to help you put what you’ve learned into action. Request your copy of the Every Victory Counts manual by clicking the button below.



















What about the elephant in the room— ED, reduced libido… in other words sexual dysfunction.
Hi A.C. Thank you for your question. Here’s a video that may be helpful: https://www.youtube.com/watch?v=bXXsh5U9G7E&t=40s (Sexuality and Intimacy for People with Parkinson’s)
I have shortness of breath almost everyday. Both my cardiologist and pulmonologist have ruled out heart and lung issues through testing. I have read that some PD patients have experienced shortness of breath. Is there something or someone that can offer a suggestion on addressing this symptom?
Hi Rosann – Thank you for reading. Some people with Parkinson’s do experience shortness of breath. For some, it is caused by anxiety. For some, it can be a symptom of their Parkinson’s medication wearing OFF. For others, as you indicated, it is due to cardiac or pulmonary issues. I recommend talking to your Parkinson’s doc about it to see if it is related to OFF times or if there may be something else going on.