If you do a quick search for images of Parkinson's online, most of the ones you’ll see are of seniors in stooped positions. But even though many believe that Parkinson's only occurs in older people (the lack of age diversity in pictures is one reason for that), 4-10% of people who are diagnosed with Parkinson’s are under the age of 50. It’s called young-onset Parkinson's disease (YOPD). While some studies define the age range as under 40 or 45, most research cites those under 50 as being YOPD.
Why does age at the time of diagnosis matter?
Very often, the emotional, social, physical, and psychological needs of those diagnosed with YOPD are different from those diagnosed at an older age. You might be soaring in your career, expecting a baby, raising multiple school-age children at home, and/or getting ready to buy your first house. These are different concerns than those who are diagnosed much later in life have.
That’s why we want to shine a spotlight on YOPD. We want you to have the education, resources, and support you need to live well with Parkinson’s no matter your age. For many, connecting with others who have YOPD is essential to their well-being; so, we've created a platform to address the most important issues people with YOPD face. With monthly live YOPD Council sessions, you will be able to ask questions and connect with others who are also defining their new normal. More about that in a bit, though. For now, let’s dive into what it’s like to be diagnosed with YOPD.
Diagnosis
When people under age 50 start to develop Parkinson's symptoms, they are often undiagnosed or misdiagnosed. Some have shared how the pain started in their shoulder, so they were referred to an orthopedist and misdiagnosed with impingement or frozen shoulder. Some experienced depression for the first time and were told it was all in their head. Their doctor prescribed an antidepressant medication, which didn't solve the issue. Some were told they were too young to have Parkinson's. While receiving a Parkinson’s diagnosis is rarely a clear process no matter your age, people who are younger often face a more circuitous path than those who are older.
Once people are diagnosed with YOPD, they often struggle with how to share their diagnosis. Because of fear of potential job implications, some choose not to tell their boss or co-workers. Some feel isolated because they don’t know anyone else their age with Parkinson's. Some withdraw completely because facing it head-on is too overwhelming. These are all normal responses to hearing news that you have a chronic and progressive disease; however, delaying the initiation of appropriate care due to all of these factors can negatively impact the quality of your life. Starting a regular exercise program, improving sleep hygiene, taking your medications consistently, connecting with others, and eating well are all undertakings you can control. More importantly, getting support from others will give you an even better chance of making sure you do.
What's different about YOPD compared to being diagnosed after 50?
Despite similarities, YOPD and a Parkinson's diagnosis after age 50 differ in clinical features and social, psychological, and emotional issues. YOPD is characterized by the typical four symptoms of Parkinson's: 1) rigidity, 2) slowness of movement (bradykinesia), 3) resting tremor, and 4) postural instability; however, the progression of these symptoms is slower. The most common initial symptoms for YOPD are rigidity and painful cramps. The most common initial symptoms for older onset Parkinson's are instability with balance while walking and tremors.
YOPD has the following characteristics: a stronger genetic component and longer survival rate, a positive response to carbidopa-levodopa (the most common medication used for Parkinson's), more motor fluctuations (ON/OFF periods), and greater dyskinesia (sudden uncontrolled movements) due to the side effects of medications.
Though each person with YOPD experiences Parkinson's differently, this table compares common clinical features of YOPD to a Parkinson's diagnosis after age 50.
| Clinical Features | YOPD | Diagnosis after age 50 |
| Progression | Slower | Faster |
| Tremor | Less common | More common |
| Rigidity | More common | Less common |
| Gait instability | Less common | More common |
| Family history | More common | Less common |
| Survival | Longer | Shorter |
| Motor fluctuations ON/OFF Periods |
More common | Less common |
| Dyskinesia Sudden uncontrolled movements |
More common Side effect of medications |
Less common |
| Dystonia Twisting, cramping |
More common | Less common |
| Depression | More common | Less common |
| Dementia | Less likely to develop | More likely |
Management of YOPD Symptoms
A variety of treatments exist to help you manage YOPD symptoms. There are many behaviors you have control over. As our founder, Davis Phinney, says, "You cannot afford to be passive in your approach, whether we are talking about your day to day management or your interaction with your health care provider."
Here are eight activities you can do today to live well with YOPD:
#1 - Exercise regularly
- Davis Phinney was diagnosed with YOPD at age 40. He exercises vigorously every day to feel better and reduce his symptoms.
- There is evidence that shows that engaging in regular moderate-intensity aerobic exercise helps slow the progression of Parkinson's.
- The earlier you start a consistent exercise program, the better you will feel physically and psychologically.
#2 - Take your medications consistently
- Your medication works best when it is at a constant level in your body. Follow your doctor's recommendation regarding the timing of your dosages.
- Watch this video and listen in as Dr. K goes into depth about the importance of medication timing.
- Read this post about protein and medication timing.
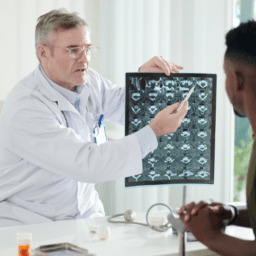
#3 - Find a Movement Disorder Specialist (MDS)
- A movement disorder specialist is a neurologist who has pursued specialized training in movement disorders. Outcomes are much better in people who see a movement disorder specialist because their doctors can customize treatment and fine-tune multiple medications.
- Click here to find a movement disorder specialist in your area.
#4 - Make an appointment with a physical therapist (PT) or occupational therapist (OT)
- One of the most common phrases we hear from people with Parkinson's is, "I wish I had seen a physical therapist sooner." Doing your daily exercise program isn't enough. Physical therapists and occupational therapists create individualized exercises that meet your specific needs. The activities they recommend can improve your posture, gait, arm swing, and other movement challenges.
- Click here to find a Parkinson’s PT in your area.
- Click here to learn why you’ll want to work with a Parkinson’s OT.

#5 - Eat healthy meals throughout the day
- Consuming a variety of foods from all five food groups provides consistent energy and keeps your immune system healthy. Focus on eating a minimum of five fruits and vegetables each day, eating a variety of high fiber foods, and staying hydrated, all of which help prevent constipation, which is often an issue for people diagnosed with YOPD.
- Watch this to learn how to use nutrition to help you live well with Parkinson’s.
#6 - Visit a speech-language pathologist (SLP)
- Since as many as 90% of people with Parkinson's experience difficulty with a raspy voice or soft speech, working with a speech therapist can help. Practicing voice exercises daily can improve your voice's quality, which can help you in your job and your social life.
- Click here to sing along to the tune "Take it Easy" by the Eagles with Davis Phinney and his daughter, Kelsey.
#7 - Learn and be open about your non-motor symptoms
- Depression, anxiety, and apathy are common in people living with YOPD. Because these topics can affect how you care for yourself, it's essential to address them with your doctor.
- Watch Dr. Pontone discuss how depression, anxiety, and apathy are managed in Parkinson's.
#8 - Practice good sleep hygiene
- Being well-rested can affect your mood and motor movements. By creating a sleep schedule, limiting daytime naps, and avoiding blue light (screen technology), you can develop habits that hopefully improve your sleep.
- Read this primer on sleep and Parkinson’s.
- Watch Dr. Postuma talk about treatment for sleep issues.
#9 - Consider Deep Brain Stimulation surgery (DBS)
- Talk with your doctor about whether you would be a good candidate for Deep Brain Stimulation. DBS is an FDA-approved surgical technique that involves a surgeon implanting a neurostimulator (similar to a pacemaker) that delivers electrical current to certain parts of the brain. When these targeted areas of the brain are stimulated, it blocks the abnormal nerve signals that cause tremor and other Parkinson's symptoms. One person with YOPD described his DBS surgery as "a buyback of life” and "daylight savings time on steroids" because he noticed such a difference in his quality of life.
- Watch this panel of DBS experts weigh in on the benefits of DBS.
#10 - Wake up and stretch
- Even if you have never tried yoga, click here for five minutes of beginner yoga with Adriene. Stretching decreases muscle stiffness and can help you feel better.
What's coming next?
Because of the unique challenges of living with YOPD, we want to increase awareness of YOPD, provide resources, and share stories to help people with YOPD live better today.
One way we’ve decided to do that is to create a YOPD Council. This council has been convened so members can share their experiences of living with YOPD. Listen in on our first YOPD Council session here.
Get to know your YOPD Council members by clicking on their names below.
- Amy Montemarano
- Cidney Donahoo
- Erin Michael
- Heather Kennedy
- Kevin Kwok
- Brian McElwain
- Michelle Lane
- Kat Hill
- Mark Kohus
How can you participate?
Register and attend our monthly live YOPD Council sessions. They will be held on the third Thursday of every month starting July 18, 2020.
We have the following topics scheduled through the end of the year:
- Sex, Love, Dating & Parkinson's (July 16)
- Work, Money, Meaning & Parkinson's (August 20)
- Disability, Insurance & Parkinson's (September 17)
- Exercise, Community & Parkinson's (October 15)
- Mental Health, Death and Dying & Parkinson's (November 19)
- Medications, Side Effects & Parkinson's (December 17)
Submit questions for the live session or other YOPD topic ideas to Melani at mdizon@dpf.org.
Where can I find more resources and information about YOPD?
World Without Limit by Alexander Andron
Old Age: A Beginner's Guide by Michael Kinsley
Talk to one of our Davis Phinney Foundation YOPD Ambassadors
Young-onset Parkinson's disease: Its unique features and their impact on quality of life
Physical activity and cognition in young‐onset Parkinson's disease
An Update on the Management of Young-Onset Parkinson's Disease
Investigation of the Treatment and Living Assistance Needed by Patients with Young-Onset Parkinson's